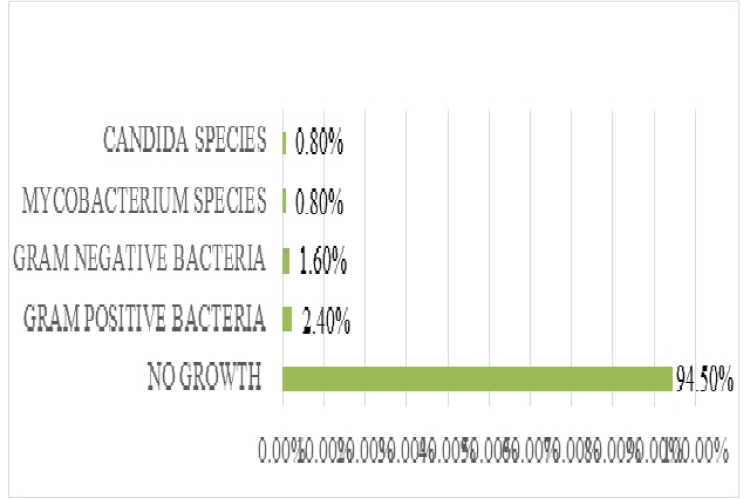
Introduction: Acute meningitis remains a serious neurological illness with significant morbidity and mortality if not treated appropriately. Effective treatment in a timely manner will minimize the poor outcome in patients with acute meningitis. It is important to identify the causative organism and its sensitivity pattern to initiate the appropriate antimicrobial therapy. It is also necessary to provide effective treatment in a timely manner to minimize the poor outcome in patients with acute meningitis. Therefore, in this retrospective study we describe the prescription pattern of antibiotics in patients with acute meningitis in a tertiary care hospital and the clinical outcome of the patients. A retrospective 5yrs observational study conducted at Lourdes hospital Ernakulam from may 2016 to April 2021. Patients diagnosed with acute meningitis and prescribed with antimicrobial agents were included in the study. (sample size 128) Results: Among 128 patients, the age wise incidence of acute meningitis was more in pediatric patients and in gender wise females were more affected. The most common type of acute meningitis seen was aseptic meningitis. Among the 7 culture positive reports, gram positive organism was found more than gram negative organism and the most commonly prescribed empirical antibiotic group were cephalosporin among which ceftriaxone is most widely used one. There were three reported ADR due to the use of vancomycin, while assessing the clinical outcome of patients, the mortality rate was 0 %. Further evaluation of clinical outcome was centered on duration of therapy and length of stay which has significant association with type of meningitis and age category respectively. Conclusion: The study shows that the early recognition of an explicit etiology that prompt meningitis, benefits in the initiation of appropriate antimicrobial therapy. This positively influence the clinical outcome.
View:
- PDF (1.44 MB)